S4E8: Fractured Neck of Femur - Geriatric EM
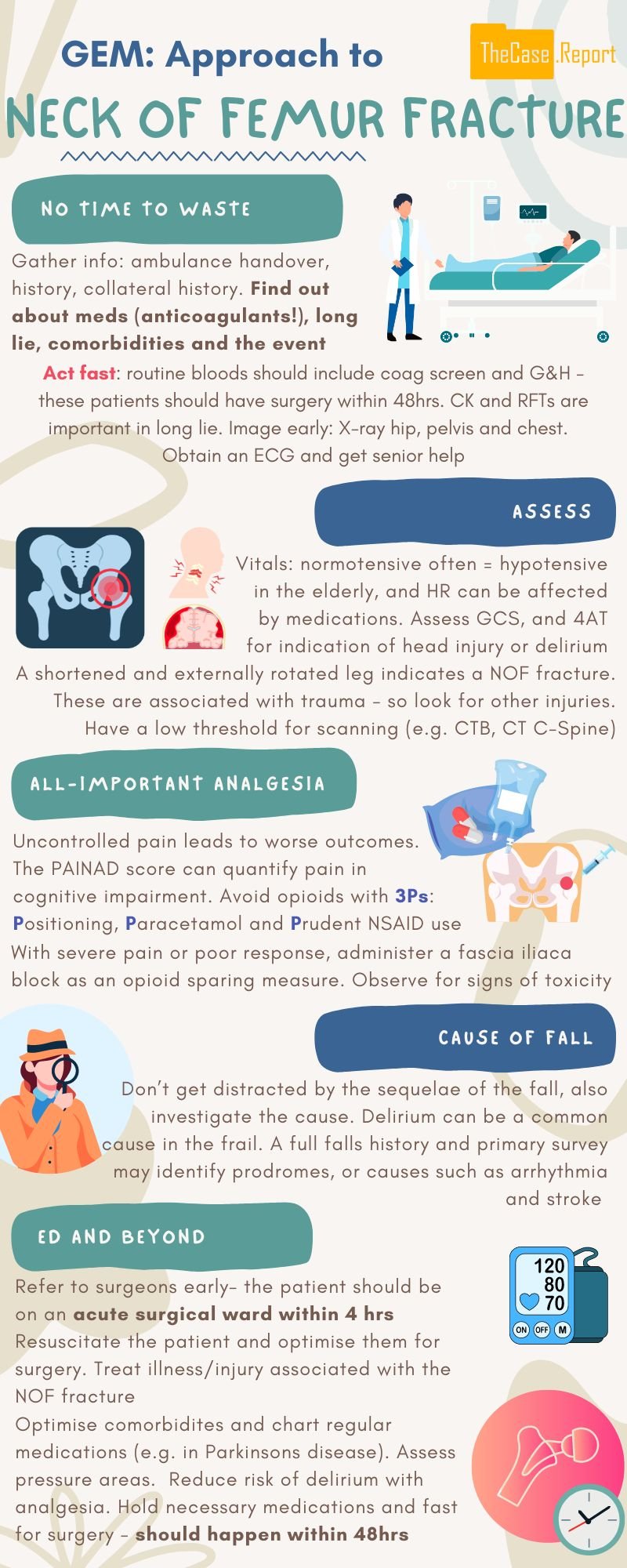
This month, the TCR team are tackling neck-of-femur fractures (NOFs). With over 3900 NOFs reported in Ireland in 2022 (1), these fractures represent a significant burden of morbidity and mortality, particularly for our older patients. Early recognition of these patients coupled with meticulous management, both in the ED and beyond, is instrumental in ensuring optimal outcomes.
Orla Kelly puts TCR newcomers Conor O’Gara and Jane Cassidy through their paces with today’s case before we sit down with our Adult in the Room - Dr Mustafa Mehmood, Consultant in Emergency Medicine in St James’s Hospital and architect of the department’s ‘Code Hip 240’ protocol.
As always, don’t forget to follow us on socials on instagram, twitter and facebook to keep updated with all things TCR. Coffee in hand? Right then, let’s get to it!
Neck of femur fractures (NOFs)
Early recognition is key
We’ve all heard of the blue book guidelines, but identifying the injury early on is key to implementing these guidelines. The typical scenario is of an older patient brought in by ambulance following a fall with a shortened and externally rotated limb. This is usually accompanied with significant hip pain and an inability to weight bear.
Key questions in the history
In this vulnerable cohort, it’s vital to know specific questions to ask, as these will affect everything from diagnosis all the way through to the patient’s management and discharge planning. Click the headings below to find out more about the types of questions to ask in a NOF/GEM history and come back later to test yourself!
Note: This is a non-exhaustive list of questions, but hits on some key points that shouldn’t be missed. Always contextualise your history based on the patient in front of you.
-
-
Address this early!
Has the patient received any pre-hospital analgesia?
-
Can the patient remember the fall?
-
If the patient cannot provide a clear history, is a collateral available?
-
Syncope/presyncope
Cardiac or neurological-sounding prodrome
Long lie
Postdrome (eg post-ictal)
Any witnessed seizure activity
-
Any history of:
Diabetes
Hypertension
IHD
Stroke
Cognitive impairment
CKD
-
In particular any anticoagulants or antiplatelets - and when were these last taken?
Any anti-epileptic or anti-parkinsonian medications due?
-
Independent vs assist of 1 vs assist of 2
Take a thorough social hx - delve into basic and instrumental activities of daily living (a little reminder of these here)
Examination
Early recognition is pertinent to ensure optimal outcomes for each patient that presents. The typical case is an older patient brought in by ambulance following a fall with a shortened and externally rotated limb. Usually they will have significant hip pain and an inability to weight bear or straight leg raise on the affected side.
It’s vital to assess the neurovascular status of the limb distal to the injury, as well as the contralateral limb for comparison, as well as paying particular attention to assessing for any evidence of compartment syndrome.
As with all trauma patients, it’s important to do a primary and secondary survey following a cABCDE approach, not focusing solely on distracting injuries. As a generally more frail cohort and given the mechanism of injury of a NOF, make sure to assess for any signs of external head injury or base-of-skull fracture. The c-spine should be cleared. If it isn’t possible to assess for midline c-spine tenderness secondary to confusion, it’s worth considering immobilisation and imaging.
A note on delirium…
As the phrase goes “all falls are mechanical” - but what prompted it? If a 4AT screen is suggestive of delirium, it’s worth considering whether it is solely due to pain, or if there are other factors at play such as infection, urinary retention, constipation etc.
Investigations
Urgent X-Ray Pelvis & Hip +/- CXR and other XRs as deemed necessary
Bloods – FBC/U&E/LFT/CRP/Coag/G&H +/- CK if long lie, troponin if any chest pain or ischaemic changes on ECG. ECG – anything suggestive of arrhythmogenic syncope or ACS?
CTB & C-Spine if deemed necessary by NICE Criteria
Urine dip & MSU if patient has urinary symptoms. Do not routinely test urine if you’re not suspicious for a UTI. Asymptomatic bacteriuria is common in older patients
Management
Common pearls and pitfalls
-
An Orthopaedic referral should be made as soon as a NOF is identified. This is so a bed on an Orthopaedic ward can be arranged concurrently with ongoing management in ED. Transfer to an orthopaedic ward should be within 4 hours of arrival to ED to ensure compliance with the 1st Irish Hip Fracture Standard (2)
-
Pain can be assessed for with a pain score at triage or PainAD score in patients with cognitive impairment. Consider Paracetamol 1g IV if pain score <2.
If the pain score >2, consider performing an US-Guided Fascia Iliaca Block (see-below), and re-assess pain regularly after giving any analgesia. If there is persistent pain despite the above interventions, consider small doses of IV Morphine (taking into account the patient baseline, condition, medications etc.)
-
Consider maintenance fluids if the patient will be fasting pre-op or if patient has had a long lie with elevated CK suggestive of rhabdomyolysis.
-
Usually a catheter is required in female patients as they will not be able to mobilise to the toilet or use a commode pre-op. However, the decision to catheterise should be weighed against the significant risk of post-op UTI.
Compliant male patients without a cognitive impairment or delirium may be able to manage with a bottle, otherwise a urinary catheter should be considered.
-
It’s always worth having antibiotics in your list of considerations when someone presents with a NOF. Look for clinical or biochemical evidence of infection, especially if you think this may be a contributing factor to a delirium.
Fascia Iliaca Block (4)
Mechanism
o Injection of long-acting local anaesthetic (LA) (usually Levobupivacaine 0.25%) into potential space between fascia iliaca & iliacus muscle - allows triple nerve blockade of the femoral nerve, obturator nerve & lateral cutaneous nerve of the thigh.
Indication
o Patients with proximal femoral fractures with significant pain at triage or uncontrolled with alternative analgesic agents e.g. Paracetamol
o Consider FIB as an opioid-sparing intervention
Contraindications
o Absolute: Competent patient refusal; LA allergy; infection over needle insertion site
o Relative: swelling around fracture site; prior femoral graft surgery; known peripheral neuropathy; recent failed FIB; patients on anticoagulants/antiplatelets
Complications
o Risk of failure 1-10%
o Haemorrhage, nerve damage & LA toxicity are less common at 0.1-0.01%
Preparation
o Obtain informed consent
o Position patient supine
o Gather equipment. Ideally your ED should have FIB Kit containing sterile drape, ultrasound cover & jelly, 2x 20ml syringes, FIB needle, drawing-up needle and a dressing. You’ll also need sterile gloves.
o Draw up an appropriate dose of Levobupivacaine 0.25% (2mg/kg, rarely exceeding 100mg)
o Ensure patient is in a monitored area e.g. Resus before and for at least 30 minutes following the procedure
Technique (5)
1. Ensure the patient has IV access, and have resuscitation equipment nearby.
2. Monitor the patient using 3-lead ECG, NIBP, SpO2, RR, and etCO2.
3. Perform a skin preparation using Chlorhexidine/Betadine, wear sterile gloves, and drape the area.
4. Use a linear ultrasound probe set to the nerve setting. Scan along the inguinal crease to identify the femoral artery, then slide the probe laterally to locate the fascia iliaca, iliacus muscle, and the fascia lata coverirg the sartorius muscle.
5. Pierce the skin using a large gauge needle.
6. Switch to a blunt-ended needle (connected via a short extension tube to the syringe of local anesthetic (LA).
7. Advance the needle, utilising a needle in-plane technique. Feel for two "pops" indicating penetration of the fascia lata followed by the fascia iliaca.
8. Aspirate again and slowly inject the LA while monitoring the patient's response, asking about sensations, and being vigilant for signs of LA toxicity or accidental nerve injection (severe pain/paraesthesia). Stop injecting if adverse effects occur.
9. After injection, withdraw the needle and apply 30 seconds of pressure distal to the injection site to direct the local anaesthetic proximally. Dress the injection site.
10. Keep patient on monitor for at least 30 minutes following FIB.
Note: As with all our material, these guides are intended for educational purposes only. Always follow local and official guidelines.
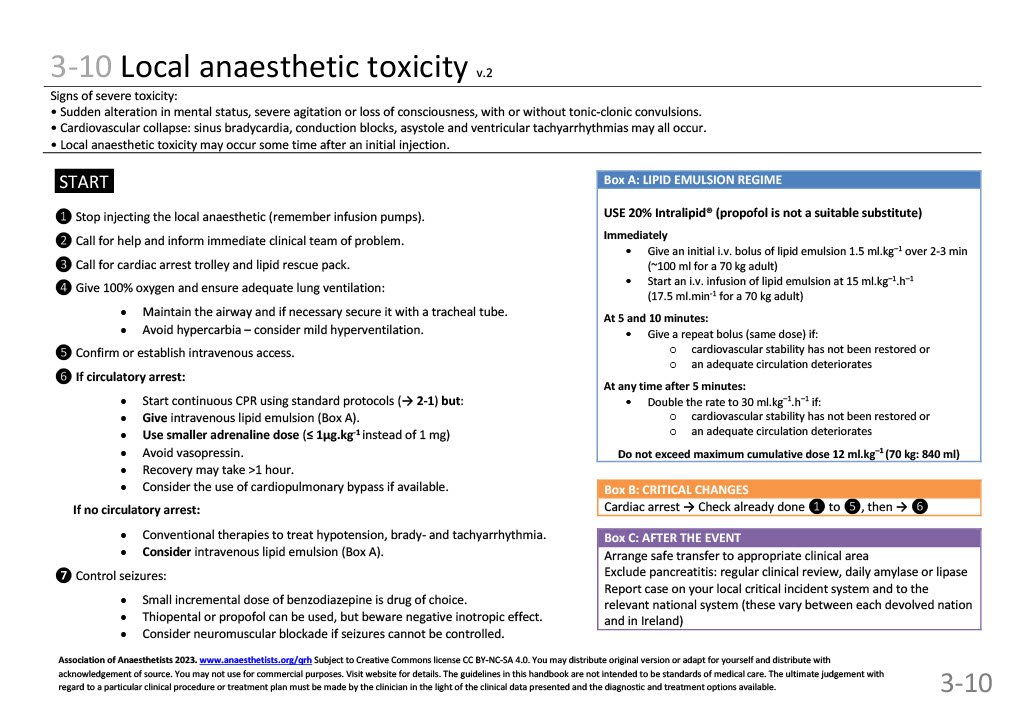
Local Anaesthetic Toxicity
This rare but life-threatening complication of FIB can occur due to exceeding the safe maximum weight-based dose or due to inadvertent intravascular injection of LA. Prevention, as always, is key. Making sure that an appropriate weight-based dosing of LA (maximum 2mg/kg Levobupivicaine 0.25%; ideally don’t exceed 40ml/100mg) is used, and using US-guided injection to reduce the risk of intravascular injection are two ways of avoiding it in the first place.
Presentation
Perioral paraesthesia is often the earliest symptom. This may be followed by abrupt changes in mental status, marked agitation, or loss of consciousness, with or without tonic-clonic convulsions. Cardiovascular collapse may manifest as sinus bradycardia, conduction blocks, asystole, and ventricular tachyarrhythmias.
June 2023 guidelines for local anaesthetic toxicity from the Association of Anaesthetists.
-
Remove the offending source - cease the administration of local anaesthetic. You should request assistance and promptly inform the immediate clinical team of the issue. Call for the cardiac arrest trolley and have the lipid rescue pack ready.
Administer 100% oxygen and ensure proper lung ventilation. Hopefully senior help has arrived at this point, and will help in maintaining the airway, securing it with an ETT if necessary.
Prevent hypercarbia and contemplate mild hyperventilation. IV access should be established if it has not already been done.
Control seizures with a small incremental dose of benzodiazepine as the preferred choice.
Consider neuromuscular blockade if seizures cannot be effectively controlled.
-
§ Initiate continuous CPR following standard protocols.
§ Administer intravenous lipid emulsion.
§ Utilise a reduced adrenaline dose (≤ 1µg.kg-1 instead of 1 mg).
§ Avoid vasopressin.
§ Recovery may extend beyond one hour.
§ Evaluate the potential use of cardiopulmonary bypass if available.
-
§ Employ conventional therapies for addressing hypotension, brady-, and tachyarrhythmia.
§ Consider intravenous lipid emulsion
EUSEM/EUGMS GeriEM Posters – an excellent resource for all things GEM! (7)
References
1. Irish Hip Fracture Database National Report 2022 https://s3-eu-west-1.amazonaws.com/noca-uploads/general/Irish_Hip_Fracture_Database_National_Report_2022_FINAL.pdf
2. Irish Hip Fracture Standards, National Office of Clinical Audit https://www.noca.ie/audits/ihfd-what-we-measure
3. IAEM Clinical Guideline - Management of Patients with Suspected Hip Fracture in the Emergency Department https://iaem.ie/wp-content/uploads/2019/04/IAEM-CG-NOF.pdf
4. IAEM Clinical Guideline - Fascia Iliaca Compartment Block for Proximal Femur Fracture in the Emergency Department https://iaem.ie/wp-content/uploads/2019/04/IAEM-CG-FINB.pdf
5. RCEM Best Practice Guideline – Fascia Iliaca Block in the Emergency Department https://res.cloudinary.com/studio-republic/images/v1635410710/Fascia_Iliaca_Block_in_the_Emergency_Department_Revised_July_2020_v2/Fascia_Iliaca_Block_in_the_Emergency_Department_Revised_July_2020_v2.pdf?_i=AA
6. AAGBI Quick Reference Handbook Section 3-10 - Local Anaesthetic Toxicity https://anaesthetists.org/Portals/0/PDFs/QRH/QRH_complete_June_2023.pdf?ver=2023-06-23-141011-603
7. EUSEM/EUGMS GeriEM Europe Postershttps://posters.geriemeurope.eu/